
Transform Your Child and Teen Clients' Lives with EMDR and Play Therapy, Healing Their Trauma for a Lifetime of Possibilities
If you are EMDR-trained and wish to effectively use it with your children and adolescent clients, register for our EMDR With Kids course. Enjoy 1-year access and a follow-up one-hour Zoom consultation.
Integrate PLAY with fidelity to the 8 phases of EMDR—because kids aren’t miniature adults. This flip chart serves as a clinical reference and an engaging visual tool, perfect for working with children and teens.
Why integrate PLAY?
-
It Is How Kids Communicate
Kids share their realities and painful stories through play, much like adults do through conversation. Whether through puppet play, turn-taking games, creating art, playing ball, or a variety of other activities, children feel safe enough to express themselves and progress through therapeutic phases.
-
Creates Safety, Making EMDR Possible
Play increases children's capacity to tolerate the stress of accessing trauma by adding essential safety, enhancing autonomic flexibility to move in and out of survival states, and supporting healthy behavior changes. This approach allows children to access more of their developing brain's potential, which is beneficial in therapy, especially to support integration.
-
Supporting Children's Healing and Development
Play, whether through non-directive "being with" or more directive approaches, supports natural therapy for children. It fosters connection, helping them overcome trauma-related isolation and reintegrate into social settings with safety. This reduces resistance, prevents them from getting stuck in survival states, and enables trauma processing without explicit discussion, vital in EMDR therapy.
"But they don't answer my questions or follow through on any of my directives. They just want to play."
Being a child therapist is challenging and exhausting, especially when working with children who have faced trauma. As an EMDR-trained therapist, you understand the importance of the 8-phase protocol, yet children and teens respond differently than adults. They express themselves through play, and their behaviors are survival adaptations. You know EMDR therapy could be transformative, but the challenge remains—how does it work with kids?
Does EMDR Therapy Work with Kids?
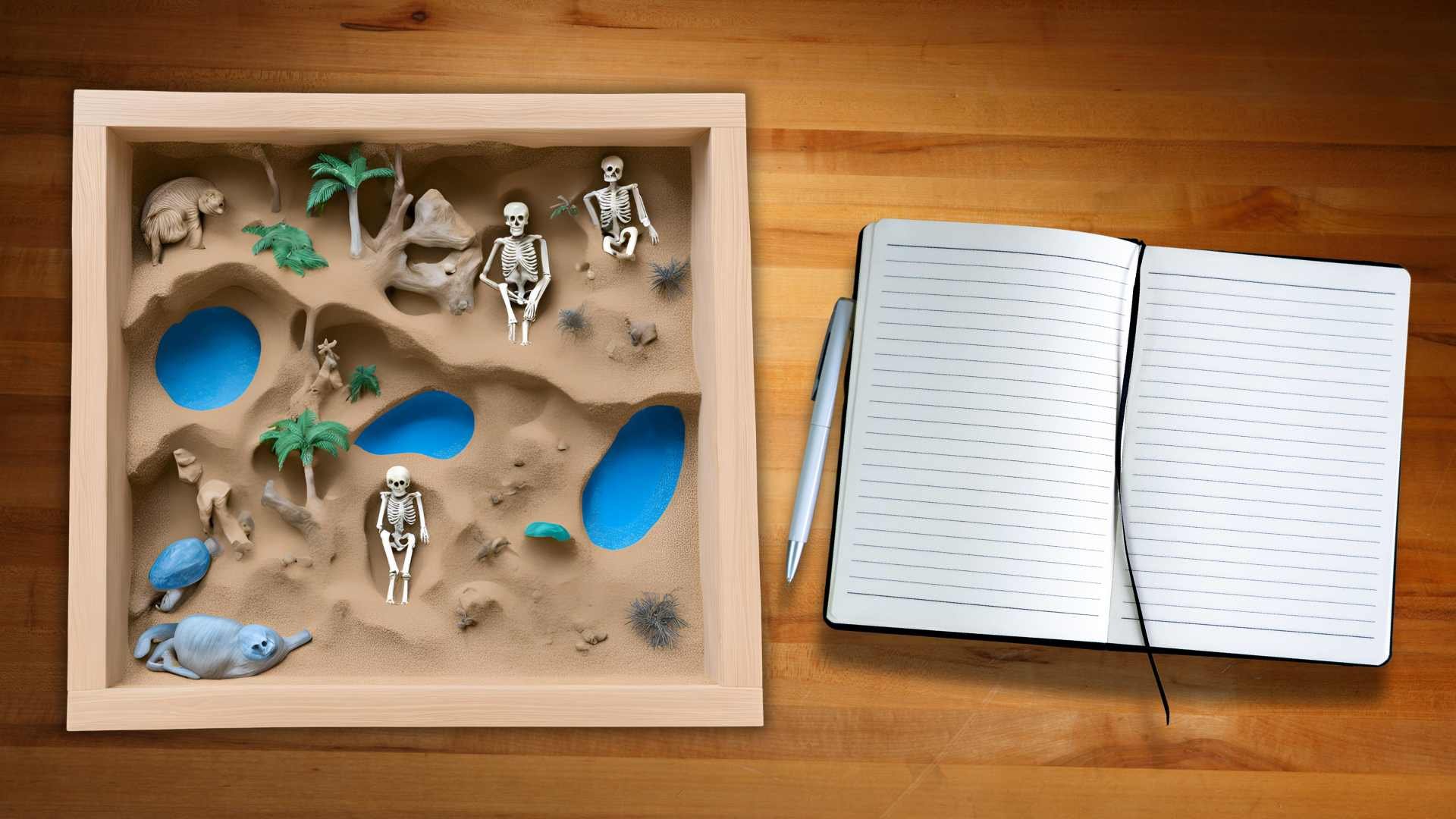
As a child therapist, your days are filled with dragon-and-dinosaur battles, turn-taking games, storytelling in the Sandtray, and playing the "bad guy" restrained with toy handcuffs to the dollhouse. Some days, you even go home and find clay in your hair from an early morning session with an 8-year-old. It feels very different from the EMDR therapy you learned to do with adult clients, making you question if EMDR is practical for kids given their developing nervous systems. You know EMDR is powerful, and you don't want to get it wrong, but moving past the preparation phase feels daunting.
What Does EMDR Look Like in Play Therapy?
Imagine being a fly on the wall in a play therapy room where a 5-year-old reprocesses trauma during an EMDR session. The child serves a small plate of toy food and the therapist, sitting on a floor pillow, responds as if they were a child, seamlessly incorporating phase 3 assessment elements. This deep attunement sets the stage for phase 4 desensitization, with natural bilateral stimulation through play. You witness how these phases, while playful and developmentally appropriate, effectively address trauma in children.
Q&A for EMDR and Play Therapy Integration
-
EMDR with children is like meeting them in their natural playground—play. When words feel too heavy, children speak the language of imagination, art, and movement. EMDR helps children reprocess their emotions by gently guiding their brain to heal, using bilateral stimulation (BLS) as a key tool. Play, in all its forms, becomes the thread that ties trauma and healing together. In my work, I’ve seen how this playful process allows children to express and release what might otherwise stay hidden, giving them room to heal and grow. It’s a safe, organic way to help children access and process emotions that are often beyond their verbal capacity.
-
Play is the heart of my work with EMDR. By blending EMDR with expressive arts, clay, Sandtray, or simply letting kids move and create, the therapeutic process becomes a dance—organic, flowing, and full of possibility. Children can externalize their feelings through tangible objects, like crafting a "worry box" or using clay to shape their emotions. The act of creating becomes a container for their inner world, holding the space for healing. In my book EMDR with Kids Flipchart and through my approach, I share how to use play as a powerful healing tool within EMDR, weaving it into every phase. Play therapy and EMDR aren’t separate—they are seamlessly integrated to create a complete healing experience.
-
Through EMDR, we provide children with a gentle yet powerful way to regulate their emotions. In Phase 2, we create a "calm place" or "container"—a safe space to store big emotions before they leave the session. I’ve found that adding play elements, like imaginative spaces or tangible items, helps children externalize and manage emotions they might not be ready to fully process. It’s all about creating that soft, grounded space where healing can unfold at its own pace, with play as the bridge between distress and calm. As children build this emotional regulation skill, they learn to control and express their emotions more effectively, both in therapy and in daily life.
-
I view resistance in EMDR therapy, including challenging behaviors, as a form of communication, rooted in the child’s nervous system. Behaviors are adaptations for survival, a way the nervous system copes with trauma and distress. As a nervous system-informed therapist, I understand that when a child resists or exhibits difficult behaviors, it often signals that more safety is needed or that the therapeutic process needs adjustment. Instead of viewing resistance as a barrier, I see it as an opportunity to offer more safety and adjust the pace of the therapy. Children’s ability to say "no" or pull back is a form of autonomy—an essential part of their healing journey. Sometimes slower progress is faster, and allowing for these moments of resistance gives the child the space they need to feel secure. I’ve found that this approach is more practical and actually increases the child’s participation in my experience. It feels safer, which leads to deeper engagement and healing. By honoring these protective behaviors and listening to them, I can adapt the treatment to better meet the child’s needs, which ultimately informs my treatment approach, fostering trust and deepening the therapeutic relationship.
-
Explaining EMDR to children is like opening the door to a new adventure. For younger kids, I keep it simple, framing it as a way to help their brains feel stronger and clearer. For older children or teens, I might describe how EMDR helps their brain "clear out old files"—a metaphor that helps them understand the processing that happens during BLS. I take great care to match the explanation to their developmental stage, always leaving room for curiosity and wonder. Parents are always involved, ensuring they understand the process, too, so they can join the child’s healing journey. The explanation is also tailored to the individual child—making it as concrete or abstract as they need it to be.
-
Item dParents are partners in the process, but I always balance that with the child’s need for their own space. I keep parents in the loop—updating them on progress, explaining the basics of EMDR, and sharing insights without overwhelming them with too much at once. The goal is for the child to feel supported by both their therapist and their parents without feeling like they’re being over-explained to. After all, healing happens when the child feels safe, understood, and free to express themselves in their own way. Parents are also encouraged to reinforce techniques at home, helping to integrate the healing process into the child’s everyday life.escription
-
For therapists new to integrating EMDR with children, I recommend starting with the EMDR with Kids Flipchart—it’s a great foundation! My upcoming book, Play IS the Therapy, dives deeper into the magic of play as a therapeutic tool. I also suggest reading Beyond Behaviors by Dr. Mona Delahooke and The Yes Brain by Dr. Daniel Siegel and Tina Payne Bryson for a deeper understanding of emotional regulation and brain development. Training in Synergetic Play Therapy, Sandtray Therapy, and the Oaklander Model is invaluable, as is learning about Polyvagal Theory and the nervous system. These resources help integrate play and EMDR effectively, building a toolkit full of creative, healing methods.
-
ItemFuture templates are like a time machine for the mind. In my work, I help children imagine and prepare for future events, guiding them through the process of envisioning how they might respond to a challenge—like a family change or school event. Play becomes part of this journey, with children role-playing or imagining themselves handling the situation with new skills and confidence. It’s a way to practice emotional resilience before the future even arrives, giving children the tools to face what’s ahead with ease. This metaphorical "rehearsal" for future challenges builds self-efficacy and coping skills. description
-
Item desMy advice: trust the process, and trust the play. Play isn’t just an activity—it’s the heart of healing. When therapists understand that play itself is a powerful therapeutic tool, they can confidently weave it into EMDR. Be flexible, be playful, and allow the child’s needs to guide the process. In my work, I emphasize that EMDR and play go hand-in-hand, creating a safe space where healing can happen organically. And don’t forget: understanding the nervous system and the power of movement is key to unlocking the full potential of EMDR with children. Integrating these playful approaches within the 8 phases of EMDR creates a truly transformative experience.cription
-
n my work, I make it a point to ensure that the materials and toys used in therapy have enough generalizability or specificity so that each child, regardless of their background, can see themselves reflected in them or create something that helps them share their own story. I believe that therapy tools should never be limiting—whether through art, toys, or play, everything should be adaptable to each child's unique cultural context. This flexibility allows children to feel seen, heard, and validated, no matter where they come from. By integrating culturally responsive materials, children can engage more deeply in the therapeutic process, helping to bridge the gap between their personal experiences and the healing work we do together.
You are not alone, and many EMDR-trained child therapists face these challenges too.
It's crucial to integrate the reciprocity of play and play-basedother opportunities for expression into the 8 phases of EMDR therapy with children while maintaining protocol fidelity. Many EMDR-trained child therapists face similar challenges. The key is to balance EMDR fidelity with the needs of a child's developing nervous system and work compassionately with parents and families, sharing information in a practical and respectful way.
In the following sections, get a glimpse of the 8 phases of EMDR with children and teens. We'll honor the developing nervous system by integrating playful approaches, including movement, expressive opportunities, shared experiences, sensory activities, and connection for a truly transformative experience.
Phase 1: History Taking and Case Conceptulization
During this phase with children, gather detailed information from parents, reports, professionals, and the child themselves. Avoid creating a cookie-cutter treatment plan, as trauma affects the nervous system uniquely for each individual. Explore trauma related to their body (e.g., medical issues, disabilities), relationships (e.g., attachment wounds, abuse), and environment (e.g., violence, safety concerns). Use play-based assessments like drawing and painting to aid communication. Build a strong therapeutic alliance and tailor treatment plans to their specific needs. Assess suitability for EMDR therapy, identify targets, resources, and potential obstacles.
Phase 2: Preparation
For this phase, the child is introduced to EMDR therapy in a developmentally appropriate way. Using animal imagery, games, and activities, the child playfully develops internal and external resources, practicing regulation skills like breath work, safe place imagery, and containment. The main purpose of this phase is to ensure the child feels safe and prepared for reprocessing. Additionally, resources for parents and caregivers are provided to support their understanding and involvement in the therapy process.
Phase 3: Assessment
In this phase, the clinician identifies a target and supports the client in activating their neural networks through play. Using metaphors, the clinician explores areas that might be inaccessible to the client. It's essential to naturally incorporate procedural steps like identifying the worst part, the image, cognitions, emotions, and the felt sense before moving on to Phase 4: Desensitization.
Phase 4: Desensitization
This phase is sometimes mistaken for the entirety of EMDR because it utilizes fast bilateral stimulation (BLS) to reduce distress. However, EMDR actually consists of eight phases, and this is just one of them. In this phase, the clinician helps the child reprocess traumatic memories through creative BLS, incorporating playful movement. Allowing the child to move naturally and playfully, rather than sitting still, makes a significant difference. Creating a shared experience can alleviate feelings of isolation. Activities like drumming, punching a bop bag, stomping, music, pool noodle fights, or alternating movements help maintain their engagement in BLS.
Phase 5: Installation
In this phase, the first step is to determine if the positive cognition identified in phase 3 still fits. The clinician then supports the child in strengthening positive cognitions related to their target, such as "I am good," "I can handle this," and "I have choices." Often, the child takes the lead in expressing these newfound beliefs, embedding them as their new truths. Methods like drawing, storytelling, playful embodiment, or role-playing are utilized to help integrate these beliefs into the child's sense of self.
Phase 6: Body Scan
In this phase, the clinician supports the child in performing a body scan to notice any lingering physical sensations, or "dust bunnies," remaining from the therapy target. Using kid-friendly body scans and playful activities like guided imagery games or simple relaxation exercises, the child becomes aware of these sensations. The clinician collaborates with the child to move through these sensations safely, using shared bilateral stimulation (BLS) or allowing movement as needed to help complete the processing.
Phase 7: Closure
This phase occurs at the end of the session. It is essential to make time for it, as it plays a crucial role in the therapeutic process. The goal is to ensure the child feels grounded and stable by the end of each session. This may involve engaging in a shared activity, such as tossing a ball, keeping a balloon in the air, picking out something from every color of the rainbow, practicing mindful breathing like dragon breaths, digging in sand using a playful container, participating in freeze dancing, or playing a favorite turn-taking game. These activities help the child return to a state of equilibrium.
Phase 8: Re-evaluation
In this final phase, which happens at the start of a return from a processing session, it's important to playfully revisit previous sessions. This helps to check the child's distress levels regarding past targets. Using play-based methods, you can assess any lingering distress from the last session, ensuring the child remains engaged and comfortable during the process.
I am thrilled to teach you how to deliver the healing power of EMDR to your clients. This self-paced course includes one year of access and a follow-up consultation hour.
Who is eligible to attend:
This training is open to clinicians who are at least partially trained in EMDR. Please note, this is and EMDRIA approved advanced course, not an EMDR Basic Training.
















